The uterus of a woman: structure, location and function. Uterus removal
To foreign bodies in the uterus include intrauterine contraceptives (IUDs) and their fragments, fetal bone fragments, and various ligatures.
Clinic. The clinical picture of foreign bodies in the uterine cavity is most often manifested by various menstrual dysfunctions (menorrhagia, menometrorrhagia, acyclic bleeding). With a long stay of a foreign body in the uterus, secondary infertility, the phenomena of chronic endometritis or pyometra are possible. A foreign body in the uterine cavity (IUD fragments) may remain asymptomatic.
Pain syndrome accompanies the perforation of the uterus of the IUD and its further migration to neighboring organs with their possible perforation. Migration of the IUD into the omentum, rectosigmoid angle of the colon, retroperitoneal space, bladder, into the caecum, to the area of the appendicular process, into the small intestine, to the uterine appendages is not excluded.
Bone fragments usually become an incidental finding in patients with menstrual irregularities, prolonged endometritis, or secondary infertility. With careful history taking, abortions are detected in a long period (13-14 weeks or more), complicated, as a rule, by prolonged bleeding, sometimes with repeated curettage of the uterine cavity.
Ligatures, usually silk or lavsan, are detected in patients with chronic endometritis and pyometra with a history of caesarean section or conservative myomectomy. These patients complain of persistent purulent discharge from the genital tract, not amenable to massive antibiotic therapy, and secondary infertility.
Diagnostics. The main method for diagnosing foreign bodies in the uterus is hysteroscopy. All the rest (ultrasound, if necessary, laparoscopy) are auxiliary.
ultrasound. The ultrasound picture of an IUD depends on its shape and type. Each type of IUD produces a characteristic and distinct echogenic image, depending on the location of the IUD in the uterus. In the optimal situation, the leaf part of the IUD is localized in the bottom, while the proximal part does not reach the level of the internal os.
With pathological displacement of the IUD its proximal part is visualized in the upper third of the cervical canal. The most serious complication of IUD is uterine perforation. It can be incomplete (the IUD penetrates into the myometrium) or complete (the IUD partially or completely extends beyond the uterus).
Fragments of the IUD can be determined both in the uterine cavity and in the thickness of the myometrium in the form of linear inclusions of sharply increased echogenicity and various sizes.
Accurate ultrasound diagnosis of bone fragments is difficult. With ultrasound, they can be determined in the form of scattered, echo-saturated structures of irregular shape.
Ultrasound with ligatures in the uterine cavity is uninformative.
Hysteroscopy. The endoscopic picture of the IUD depends on its type and the time of the study. With a long stay of the IUD in the uterus, it is partially covered by synechia and endometrial flaps, salt crystals. Perhaps the formation of bedsores on the wall of the uterus. If fragments of the IUD are suspected, hysteroscopy should be performed in the early phase of proliferation, carefully examining all the walls of the uterus. Fragments of the IUD can be the remains of a crushed plastic part, metal fragments, "whiskers" and can either be freely located in the uterine cavity or partially embedded in its wall. If perforation of the uterus of the IUD is detected, hysteroscopy is performed in conjunction with laparoscopy.
Hysteroscopy is performed when fragments of the IUD remain in the uterine cavity due to its unsuccessful removal and there is a suspicion of perforation of the uterus of the IUD. Prolonged stay of the IUD in the uterine cavity sometimes leads to its dense attachment and even ingrowth into the thickness of the myometrium. Attempts to remove IUD fragments in such situations have been unsuccessful. Hysteroscopy allows you to determine the localization of the IUD itself or its fragments and accurately remove these foreign bodies.
The hysteroscopic picture of bone fragments depends on the duration of their stay in the uterus. If the period is relatively short, then lamellar dense whitish formations with sharp edges that have penetrated the wall of the uterus are visible. When you try to remove them, bleeding often begins. If the bone fragments have been in the uterine cavity for a long time (more than 5 years), they have a characteristic crystalline structure (coral-like shape) and, when they are removed with forceps, they crumble “like sand”. Bone fragments are more often located in the region of the mouths of the fallopian tubes and the bottom of the uterus.
Ligatures during hysteroscopy are defined as whitish threads against the background of general hyperemia of the uterine mucosa in its lower third along the anterior wall (after cesarean section) or in various areas (after conservative myomectomy)
Treatment. Foreign bodies are removed from the uterus during hysteroscopy using special endoscopic instruments. It is not recommended to try to remove the IUD without visible "whiskers" blindly, with various devices. Such attempts usually result in deformity and fragmentation of the IUD, and sometimes perforation of the uterus. If uterine perforation is suspected, the IUD is performed jointly by hysteroscopy and laparoscopy.
If, according to ultrasound data, fragments of the IUD are determined in the thickness of the myometrium, and they cannot be determined during hysteroscopy and laparoscopy, one should not try to extract these fragments from the thickness of the wall. Further monitoring of the patient is necessary.
In the postoperative period after removal of a foreign body from the uterus, antibiotic therapy is recommended, taking into account the sensitivity of the flora to the drug.
Instead of an introduction
"If youth knew, if old age could"(proverb)
“You see, yesterday I left the operating room in a good mood,” a familiar gynecologist told me, “the operation was not difficult, but delicate. All that was needed was nothing: to remove the overgrown part of the fallopian tube, and to transplant its healthy remnant into the corner of the uterus.
At that not so distant time, there were still no “high technologies like IVF” and gynecologists associated the opportunity to make happy a woman exhausted by infertility with overgrown openings of the fallopian tubes with the plastic restoration of their patency.
- The operation was successful, I think that the patency will be restored and, perhaps, the patient will fall into those 70% of pregnancy that the PVM had (Chief's initials).
Today, the problem of surgical treatment of tubal infertility has “gone” into the background. But there was a time when the leading specialists of the clinics "competed" in achieving the best results.
- And so, in this good mood, I go into the staff room and, what would you think? I see the Calendar Year there! Twelve female employees who came running for a short lunch break. In terms of faces, characters, work experience, and experience, this is what your 12 months are. On the tables between the case histories are tea cups, homemade sandwiches and other lunchtime victuals. And all at the same time they are talking animatedly about something. January, February, March glanced at the creaking of the door. To my brief "Salute!" They looked around in surprise and continued their serious conversation, not understanding my mood. Taking the operating log, he settled on the couch and, concentrating, began to describe the operation performed. Naturally, I involuntarily listen to a peaceful conversation, and oh God! What would you think they were talking about? About bras. For a moment it seemed that I was not in a 140-bed clinic, but in a women's clothing store. The hand trembled and began to unsteadily display the progress of the operation. Phew - you! He tried to change the course of a business discussion by asking loudly: who read the latest issue of Obstetrics and Gynecology? April, May, June turned around and, sipping tea, looked at me as if I were an empty place. July asked: “What is interesting there?” August, fighting and fast, retorted: "Solomatin must be read!" September, October, November got up and, while chewing, said: “Homo sapiens, it’s better to go down to us, to the delivery room, there you will see everything that is written in your journal.” And even December, the 72-year-old Veteran Doctor, who was sitting by the window and correcting the flaws of all Eleven in the case histories, raised her head, silently looked around at everyone and again delved into her work, which allowed her to submit medical documentation without delay. statistics.
“By the way,” he asked, “have you read Solomatina?”
“No, I didn’t read it,” I answered, “but what?
- They say that he writes interestingly, and everything about our brother, obstetrician-gynecologists.
Intrigued, I looked online. And there ... "Tatyana Solomatina - candidate of medical sciences, in the past an obstetrician-gynecologist ...". And a list of books.
I hold in my hands "Obstetrician-Ha!". Evil, but good. He sneers, but there are also sober thoughts. From the review of journalist Y. Vasiliev: “ Thanks to this book, you will take a fresh look at familiar things: doctors and patients, illness and recovery, the problem of fathers and children, life and death ... ".
The chapter "First Night" begins with the words: "Getting a medical specialty is not so easy." Smart and… fascinating. The chapter ends: P. S. And the doctor, in addition to attentiveness and not squeamishness, materialism and superstition, faith and disbelief, communion with the sacraments of life and death, is characterized by speed of reactions, like fighter pilots or special forces officers who capture secret military points deep behind enemy lines.
That's it, and you're talking about bras.
I turn the page, the next chapter is "Glory to Russia." It turns out that this is addressed to glassblowers. A short, only 2 page story, but it got me thinking.
The essence of the story in a playful presentation of a very serious gynecological issue of foreign bodies. The patient complained of urinary incontinence. Upon questioning, it turned out that two or three years ago she was recommended to measure the temperature in the vagina. She took the thermometer and fell asleep. When I woke up I couldn't find the thermometer. There were no disturbances. She got pregnant, gave birth, was healthy. And now, after several years, doctors cannot establish the cause of dysuric disorders. Thanks to the ultrasound, they found a foreign body in the bladder. It turned out that an ordinary, completely intact glass mercury thermometer, which suddenly disappeared three years ago, was lying in the bladder. A funny episode, but leads to a sad thought.
From memories
"All stupid things on earth are done with a smart face"(Baron Munchausen)
Episode 1. As a student of the 6th year, the leading teacher, associate professor Nikolai Viktorovich Andrezen, led us subordinators to the educational museum of the department during the passage of the topic "Abortion". This museum was founded in the clinic in the second half of the 19th century by Professor KF Slavyansky and was constantly replenished. In it, among numerous macropreparations, he showed us a "set" of objects extracted from the genital tracts of women that got there in various ways, most often during criminal abortions.
The picture is impressive (Fig. 1).
Fig.1 A set of objects taken from the genital tract.
On the recommendation of the associate professor, I go to the library, open the book by M.G. Serdyukov “Forensic gynecology and forensic obstetrics” and on page 291 I read: “ It goes without saying that the presence in the genitals in the presence of pregnancy or during abortion of various foreign bodies " (pieces of bougie and rubber tubes, plant roots, pieces wood, fragments of a crochet hook, remnants of fabric or rope, and in one rare casuistic case, a woman giving birth inserted a medical thermometer into her uterus for the purpose of abortion) serves as an indication of an abortion.
And he gives two examples. In one of the abdominal cavity, Gegar's dilator No. 5 was removed, which got there during a criminal abortion made six months ago. In another, "... a twig from a broom wrapped in gauze, 19 cm long and 0.5-0.3 cm thick in different parts(p. 292).
A few years later, he gained his own experience in extracting a foreign body from the uterus.
Episode 2 While already in graduate school, he worked part-time on weekends and holidays in the so-called "septic gynecological department". Once, as usual on Sunday, at 9 oo I took over for duty. The morning was calm, there were no emergency patients. I made a leisurely "introductory" round, talked with the patients and, having finished, got a job in the staff's room with my dissertation affairs. After a while, one of the women in the department comes in and, embarrassed, says that she wants to tell something. Invited to sit. I took a medical history and found out that she had been in the hospital for two days. Was admitted on Friday with a diagnosis of feverish spontaneous threatened abortion during pregnancy 10 weeks. There is no bleeding, and the temperature is high up to 38 o -39 o, therefore, it was observed while conducting antibiotic therapy.
- Tell me.
- Upon admission, I was embarrassed to say about the intervention for the purpose of abortion.
“What kind of intervention is this?” I asked her, who turned out to be a nurse in one of the hospitals.
Doctor, this is not my first abortion. I have always called it the introduction of a hairpin. She took it by the ends, and inserted it into the cervix with a blunt end. And everything was fine. And this time the hairpin slipped into the uterus.
- "Here's your grandmother and St. George's day," I thought, - a calm morning quickly ended. As the hero of the movie "Liquidation" said: "Oil painting." As they say today, the algorithm of action was clearly marked in my head: x-ray → clarification of the diagnosis → further decision.
I called 03, explained the situation, asked for assistance, and in 5 minutes I received an answer: an on-duty traumatology unit with an X-ray machine at the other end of the city. Well, the day is long. I ask for understanding and help. They sent a "transportation", took it, did it, brought it back with a picture. Here it is dear, as in the palm of your hand, lies across the uterine cavity: the curved part to the right, the tips to the left.
Next is the matter of technology. Under local infiltration anesthesia with a 0.25% solution of novocaine, paracervical, 120 ml, dilation of the cervical canal to No. 12, careful entry into the uterus with a long Kocher forceps, groping, grasping and leisurely removal of the hairpin (Fig. 2). Then excochleation ovi and abrasio cavi loss. The patient was discharged the following day in a satisfactory condition.
Fig.2.
 When he reported this clinical observation at a meeting of the Society of Obstetricians and Gynecologists in Kazan, Mark Iosifovich Slepov, Associate Professor of GIDUV, spoke in the debate and said:
When he reported this clinical observation at a meeting of the Society of Obstetricians and Gynecologists in Kazan, Mark Iosifovich Slepov, Associate Professor of GIDUV, spoke in the debate and said:
You were lucky, there was a metal object. But I suffered in a similar situation, removing a glass eye stick from the uterus. I just thought about how not to crush it into pieces. But everything went well.
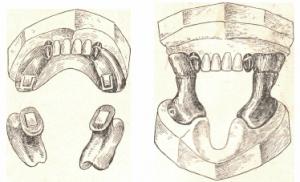
Or it may not be possible and you will have to resort to surgical intervention. In the museum of the department there is an exhibit under No. 114, which is a fragment of the tip of Brown's syringe (Fig. 3). The accompanying inscription says that Dr. V.V. On March 24, 1923, Dyakonov had to cut the cervix to the internal os, and only then was it possible to remove the foreign body from the uterus.
Fig.3. Brown Syringe Tip Fragment
 The moderator of the meeting, Professor Pavel Vasilievich Manenkov, recommended to "look" into the "Course of Obstetrics and Women's Diseases" by prof. V.S. Gruzdev. The chief's instructions must be followed.
The moderator of the meeting, Professor Pavel Vasilievich Manenkov, recommended to "look" into the "Course of Obstetrics and Women's Diseases" by prof. V.S. Gruzdev. The chief's instructions must be followed.
I open the first part of "Anatomy and physiology of the female reproductive apparatus" (M., 1919) and on page 14 I read: “... the female urethra differs from the male urethra in its long, lumen width and especially extensibility: the length it is only from 3 to 4 cm, and the extensibility is so significant that the urethral canal can easily be stretched with bougies to a diameter of 1 cm and even so much that an index finger can be inserted into the bladder.
Today, against the background of existing methods for examining the bladder, the examination of its walls through the dilated urethra is completely forgotten. For this, there was a special set of Simon's mirrors. Here is what V.F. wrote about this. Snegirev (Uterine bleeding. M., 1895, 2nd edition, p. 34): “... star-shaped shallow incisions are made on the external urethra, penetrating through the mucous and muscle tissue and gradually begin to insert mirrors from a smaller number to a large one. Already at No. 6, the urethra is so dilated that you can easily pass your index finger through it, and at No. 7, under artificial lighting, it is easy to seeper visumwith the color of the mucous membrane of the bladder or neoplasms in it.
I open the second part of "Obstetrics" (Berlin, 1922, volume 2) and on page 209 I read: “Introduction into the uterus of bougie, etc. objects is a favorite method resorted to by “specialists” and “specialists” in criminal miscarriages ... in the villages, tools such as spindles are used for this purpose ... In my practice, there was a case where a peasant woman, trying to insert a spindle into the uterus, pierced in several placesseptum vesico— vaginale, causing the formation of several vesicovaginal fistulas; however, she did not succeed in terminating the pregnancy, subsequently she was safely relieved of the burden on time, and a few months later all her fistulas were sewn up by me.
I open the third part of "Gynecology" (Kazan, 1922) and on pages 90-91 in the section on diagnostic methods I read that " X-ray studies could be successfully used in gynecological practice ... for the recognition of metallic foreign bodies in tissues and organs " in cases where “... the correct diagnosis is extremely difficult, due to the reluctance of patients out of a sense of shame to reveal to the doctor the true cause of the disease. I myself once had to remove from the bladder of a young girl, through a previously dilated urethra, a head pin, which was strongly bent and caused unbearable suffering to the patient (Fig. No. 64). Undoubtedly, the patient herself put the hairpin there, masturbating; nevertheless, both before the operation and after the removal of the hairpin, she stubbornly continued to deny this.
The hairpin from Prof. V.S. No. 1. Well, how? Have you arrived?
And further. In the section “Traumatic injuries of the female genital organs” (pp. 195-203), Prof. V.S. Gruzdev devoted three pages to injuries associated with foreign bodies. He's writing: “A relatively common source of traumatic injuries of the genital apparatus in women are the so-called. "foreign bodies", which are most often found in the sleeve, less often - in the uterus, bladder, parts of the abdominal cavity adjacent to the genital area, etc. ... The purposes for which they are introduced are varied ... These bodies themselves are extremely diverse ... various instruments , pessaries (often home-made), hysterophores, bougies, head pins, knitting needles, corks, balls of thread, wooden balls, wine glasses, fondant jars, coils, candlestick heads, cow horns, etc., etc. ” (Gynecology. Kazan, 1922, 1st edition, p. 199).
And further (NB!). “Remaining in the genital canal, bladder or abdominal cavity, sometimes for whole years, even tens of years, foreign bodies can, in the end, have a strong irritating effect on the walls of the vagina, bladder, etc., can then penetrate into the thickness of these walls and, finally , perforate them. Moreover, on this basis, fistulas can occur - vaginal-vesical, vaginal-rectal, etc.(ibid.).
An example of "creativity and diversity" is exhibit No. 95, stored in the museum of the department. This is a piece of dry reed (Fig. 4).
Fig.4.
 Judging by the explanatory text, “grandmother’s instrument for inducing a miscarriage” was delivered to the museum of the department by Dr. V.S. Kandaratsky, who, while working as an emergency doctor, in 1926-1928 was a freelance intern for prof. V.S. Gruzdev.
Judging by the explanatory text, “grandmother’s instrument for inducing a miscarriage” was delivered to the museum of the department by Dr. V.S. Kandaratsky, who, while working as an emergency doctor, in 1926-1928 was a freelance intern for prof. V.S. Gruzdev.
And we find a completely “exotic” description of criminal abortion in another student, prof. V.S.Gruzdev - intern I.V.Danilov (future professor, head of department, director of GIDUV). Here is its essence. To a 24-year-old woman, a “grandmother”, in order to terminate a pregnancy of about 3 months, introduced a goose feather into the uterus. The insertion "... lasted a long time and was painful." She tied the outer end of the pen with a harsh thread to her right thigh. For three days the woman was at home. There was no miscarriage. On the 4th day, due to chills and severe bleeding from the genital tract, she went to the hospital. Having examined it, Ivan Vasilievich did not find a pen, and the thread went into the cervical canal. It was not possible to extract the feather by pulling it, and per rectum it was found in the back Douglas "... a solid body, in the form of a stick, as thick as a finger." By scraping the uterine cavity, he removed the fetal egg and at the same time revealed a perforation on the posterior wall of the uterus. Emergency cutting. A goose feather 9.5 cm long and a thread 70 cm long were removed. There was no damage to internal organs. The hole in the uterus is sutured. Recovery (Kazan medical journal, 1931, p. 907-908). For other details, see our methodological manual "Perforation of the uterus" (Kazan, KSMU, 2000).
By the way, in connection with the issue under consideration, we strongly recommend reading the book by L.E. Ulitskaya - "The Case of Kukotsky" (M., 2004).
Episode 3 One day a young woman, virgo, came in complaining of foul-smelling vaginal discharge, which appeared, in her words, "out of the blue." During the examination, we were lucky: the hymen turned out to be easily stretchable and the hole in it freely passed the index finger. I palpate some kind of soft formation resembling cotton wool. With a long Kocher clamp, I carefully grab the lower pole of it and freely pull it out with a slight pull. Ba! Yes, it's a swollen sanitary tampon. The patient was embarrassed and remembered that she had used it not so long ago, but believed that she removed everything in a timely manner. Washing the vagina with a weak solution of potassium permanganate, followed by a dose of olazol, completed the procedure.
Surgery met the end of the 19th and the beginning of the 20th century with the introduction and development of asepsis and antisepsis. In Kazan, prof. V.S. Gruzdev after prof. N.N. Phenomenov actively used surgical methods for the treatment of gynecological patients. In this regard, a new problem has arisen: foreign bodies forgotten in the abdominal cavity during surgery.
Joke. In the old days, the professor finished the operation on the abdominal cavity, changed his clothes and was anxiously looking for something, holding the bridge of his nose.
Operating room nurse - What have you lost, professor?
Professor - Pince. Can't remember where it might be?
Operating sister (jokingly) - In the abdominal cavity of the patient, professor.
Professor - Really? Urgent x-ray! This is true.
Prepare for relaparotomy.
A joke is a joke, but the matter is very serious even today.
Throughout the 20th century, publications about such incidents periodically appeared, and even now there are publications. So recently, in a popular publication, it was reported that during the control at the airport, one lady had a metal object forgotten in the abdominal cavity during an operation performed several years ago.
Prof. V.S. Gruzdev drew attention to this problem at the very beginning of his activity by publishing the article “On the issue of foreign bodies in the abdominal cavity and the attitude of the peritoneum towards them” (Russian doctor, 1906, No. 30, p. 917), soon reprinted in German. A few years later, in his "Course", he returned to this issue in the section on traumatism of the female genital organs: " among the foreign bodies of the abdominal cavity that the gynecologist has to deal with, the majority are instruments, gauze compresses, etc. objects introduced here during abdominal-mural abdominal dissections and then forgotten here ...
I myself once had to remove a clamp through the vaginaTerrier, at 22 Sept. long (Fig. 150), forgotten in the abdominal cavity after ovariotomy ... the instrument remained in the abdominal cavity for 7 years ... After examining, I made sure that the patient's stomach was, in a clamped form, a long instrument, the top of which, having perforated the abdominal wall, came out sant. 2 above its surface, while the handle is palpable in the posterior vaginal fornix. Removal of this instrument by posterior colpotomy was relatively easy for me, and 2 weeks later the patient was quite healthy."(Gynecology. Kazan, 1922, 1st edition, p. 199). The removed clamp has been kept in the museum of the department for more than 100 years as a visual aid (Fig. 5).
Rice. five.
 This question worried him all his life and he drew public attention to it for the third time in the publication “On the issue of the responsibility of gynecologists and surgeons for leaving instruments and other objects in the abdominal cavity of patients during abdominal surgery” (Kazan medical journal, 1926, No. 2, p. 215).
This question worried him all his life and he drew public attention to it for the third time in the publication “On the issue of the responsibility of gynecologists and surgeons for leaving instruments and other objects in the abdominal cavity of patients during abdominal surgery” (Kazan medical journal, 1926, No. 2, p. 215).
We have seen a similar incident.
Episode 4
“No, life is not only a May day,
Where everyone dances and sings ... "
(from song)
In 1989, in December in Kazan, on the initiative of the Ministry of Health of the TASSR, KSMI, the Republican Clinical Hospital and the Scientific Society of Therapists, a republican scientific and practical conference was held on the problem of "Medical errors: causes, ways to overcome." "Abstracts" of reports (Kazan, 1989) were published. In the fifth section "Obstetrics and Gynecology", the curious Reader will find our publication "Timely diagnosis of foreign bodies in the abdominal cavity during caesarean section" (pp. 156-159). It outlines the circumstances and medical tactics in two observations. Here is their essence.
Observation 1. A 34-year-old pregnant woman had an emergency caesarean section. Under general endotracheal anesthesia, a boy 3200 gr. During the suturing of surgical wounds of the uterus and abdominal wall, the anesthesiologist asked to speed up the operation due to the lack of narcotic drugs necessary to continue anesthesia, because. the matter was coming to an end. After the application of skin sutures, the surgeons, due to the haste that arose, suspected the abandonment of napkins in the abdominal cavity, which were placed in it for isolation before removing the fetus. The operating sister confirmed the fears of the surgeons, but unfortunately, after suturing the abdominal wall. An ultrasound was urgently performed to confirm: "there is a homogeneous shadow in the lateral parts of the abdomen." They resorted to urgent laparoscopy - gauze pads located behind the uterus were found; retrieved. Postoperative period without complications.
Observation 2. A 32-year-old woman in labor underwent a caesarean section during the third urgent delivery due to the persistent weakness of labor. In the postoperative period, the phenomenon of intestinal paresis for 9 days. The treatment was carried out with varying success. The suspicion of leaving a foreign body by the operating doctor was categorically rejected. Laparoscopically on the 9th day revealed the presence of such. Relaparotomy. Removed the diaper introduced into the abdominal cavity to isolate it before removing the fetus. The doctor who was present at the relaparotomy, who performed the caesarean section and being sure of complete sinlessness, fainted. Protracted postoperative period, discharged on the 21st day.
The conclusions are as old as eternity: in order to prevent the abandonment of a foreign body during abdominal surgery, there should be maximum mobilization of the attention of the surgeon, his assistants and the operating sister. At the slightest suspicion, an immediate clarification of the diagnosis is necessary. Neglect of this leads to severe complications, delayed removal of a foreign body and a protracted postoperative period.
Episode 5 Let me tell you about another case from personal experience. Once I had to operate on a familiar patient with a large cystic tumor, the upper border of which was at the level of the navel. For safety net and greater confidence, I asked assistant professor I.F. Polyakov. By opening the abdominal cavity, it was determined that it was a giant parovarial cyst (the macropreparation is stored in the museum of the department). Its enucleation was associated with the exposure of an extensive interligamentary surface, on which there were multiple punctate bleeding areas. There was no electrocoagulator. I used small gauze swabs, taking several pieces at the same time in my hand and pressing them to the bleeding areas. Ivan Filippovich reminded me several times that such small tampons should be taken with clips, because you can lose them in the abdominal cavity. I deliberately went to the violation of this installation. It was inconvenient to use a large gauze pad in this particular situation, and one tampon on the clip was not enough. Accepting the remarks of the assistant, I asked him to increase vigilance. He himself tried to hold these tampons in his fingers as tightly as possible. Before suturing the abdominal wall, we carefully examine the abdominal cavity. And what do you think? We found one after another three (!) small gauze tampons lying freely in different parts of the abdominal cavity. I think comments are unnecessary. At that moment, I was ashamed and looked with gratitude at the silently looking at me, a wonderful friend and assistant - Associate Professor Ivan Filippovich Polyakov. It is pointless to talk about further experiences. The postoperative period passed without complications. I breathed a sigh of relief only after the patient was discharged home. The woman lived for a long time and, already at an advanced age, died from a severe extragenital disease. Grateful to colleagues. The secret of negligence was delicately preserved. Although they say that the winner is not judged, however, it is impossible to avoid self-condemnation. Self-flagellation is not the best thing. Today this secret was revealed for the first time for you Dear Reader. You want to judge, you want to have mercy.
Episode 6 Above, we have already talked about the possible long-term, for years, presence of a foreign body of the uterus in the abdominal cavity. Outcomes are varied. Several such observations took place in the clinic of prof. V.S. Gruzdev.
Observation 1. The woman was admitted with a diagnosis of recurrent ovarian tumor. From the anamnesis it was established that about two years ago she was operated on at the place of residence for an ovarian cyst. The postoperative period was complicated by infiltration at the site of the removed tumor. Conducted therapeutic measures "significantly reduced the size of the infiltrate." Throughout the year she felt satisfactory, but recently she began to feel pulling pains in the right iliac region. She turned to a gynecologist, who discovered an immobile tumor-like formation in the region of the right appendages and sent the patient to Kazan. During the examination, it was found that to the right and somewhat behind the uterus there is a rounded, with clear contours, slightly painful, dense, immobile tumor, resembling an ovarian fibroma. ventiotomy. Extensive adhesive process, which made it difficult to remove the tumor. The latter is 12x15 cm in size. On the cut: a dense, thick, up to 1 cm pseudocapsule, a gauze napkin lies in the cavity. Recovery. The macropreparation is preserved in the museum of the department (Fig. 6)
Rice. 6.
 When this observation was reported at a meeting of the Scientific Society of Obstetricians and Gynecologists, prof. N.E. Sidorov shared his experience of removing a gauze pad from the bladder in the debate. She was forgotten in the abdominal cavity during the operation to remove the tumor. Over time, a bedsore formed in the wall of the bladder, and a napkin found during cystoscopy penetrated there.
When this observation was reported at a meeting of the Scientific Society of Obstetricians and Gynecologists, prof. N.E. Sidorov shared his experience of removing a gauze pad from the bladder in the debate. She was forgotten in the abdominal cavity during the operation to remove the tumor. Over time, a bedsore formed in the wall of the bladder, and a napkin found during cystoscopy penetrated there.
And one more thing, about forgotten napkins from the story of Associate Professor V.I. Zhuravleva:
A year after the caesarean section, a woman with suspected foreign bodies in the abdominal cavity was delivered to the gynecological department of the Republican Clinical Hospital of the Ministry of Health of the Republic of Tatarstan at the place of residence. During the examination, clearly visible protrusions of the anterior abdominal wall were found in the epigastric region symmetrically from the midline close to the costal arches. On palpation, they give the impression of the presence of infiltrates, and ultrasound revealed foreign bodies. A surgeon was invited - associate professor V.V. Fedorov. A collective decision was made to proceed with surgery. Since the infiltrates were intimately connected with the anterior abdominal wall, they limited themselves to dissection of the abdominal wall above them without entering the abdominal cavity. Removed two napkins 20x20 cm. Further anti-inflammatory treatment. The outcome is recovery.
Observation 2. The woman was admitted 8 months after surgery for an ectopic pregnancy complicated by postoperative infiltrate in the posterior Douglas space. Treatment at the place of residence remained without effect. At that time, I was mastering the treatment of inflammatory processes and she was put in my ward. During the examination, there really was an infiltrate behind the uterus of a “woody” density, moderately painful, without clear boundaries, approximately 7x8 cm in size. When puncturing through the posterior fornix, there was a feeling of “entering the cartilaginous tissue”. No content received. Within a week, anti-inflammatory therapy was carried out. Naturally without success. After a week of observation, Prof. P.V. Manenkov recommended a second puncture with a larger diameter needle. Frankly, I doubted the need for such, since not only fluctuations, but even a hint of some kind of softening of the infiltrate was not. However, the appointment must be made. The operating sister prepared a syringe with a thick needle, which I passed into the infiltrate as deep as possible. Sipping the plunger and at the same time slowly withdrawing the needle completed the procedure. The syringe is empty. But what is it? Is there any thread on the tip of the needle? Truly "there would be no happiness, but misfortune helped." I carefully examine and find a barely noticeable notch on the tip of the needle, which hooked and removed the thread from the bowels of the infiltrate. And then “like a bolt from the blue” it dawned on me: a napkin! Then it's a matter of technique: colpotomy, removal of a napkin 20x20 cm, anti-inflammatory therapy, recovery. The patient was discharged with recommendations to continue rehabilitation at the local resort of Bakirovo.
Observation 3. And yet, in connection with an ectopic pregnancy. The woman was admitted two months after the operation with an infiltrate in the stump. During the examination, he found a dense infiltrate without clear contours, dense, 6x7 cm, slightly painful, to the left and behind the uterus. Prof. P.V. Manenkov on the round, having carefully weighed all the circumstances of the case, and especially the fact that the woman had been continuously receiving anti-inflammatory therapy at the place of residence for two months without any effect, recommended abdominal surgery due to suspicion of a foreign body. I was entrusted with doing it. Opened up the abdomen. I carefully separate the adhesions and find nothing but "cartilaginous density". Pavel Vasilievich stood nearby and gave advice. My indecisive actions brought him out of patience and, taking a long probe, he began to poke it in different areas. And in one place it suddenly fell deep into the infiltrate. It turned out to be a cavity 1.5x2 cm, in which were two silk ligatures and a small amount of turbid liquid, which turned out to be sterile during an urgent laboratory examination. Sanation. Suturing. Recovery.
"Not there"
We have already quoted Prof. V.S. Gruzdev about the great extensibility of the female urethra. Here's another one: More than once I have seen married women with a congenital absence of a sleeve, who, without any special disorders, apparently had sexual intercourse through an enlarged urethra.". (“Course of obstetrics and w.b.” M., 1919, part I, p. 14).
Everyone who is more or less interested in congenital absence of the vagina or colpopoiesis is familiar with the work of prof. B.V. Sherstnev on colpoelongation. With the help of the device he invented, he managed to obtain a sufficient deepening of the tissues of the vestibule of the vagina and the adjacent zone due to their extensibility and thereby create conditions for coitus. A similar situation can occur in natural conditions. So in Kazan honey. well. (1926, v.2, pp. 209-210) an article by L.N. Sobolev "A case of 16-year-old sexual life in the absence of a vagina and uterus". Word to the author. " The patient got married at the age of 21. Firstcoituswas without pain and blood and, apparently, failed ... this went on for 2-3 years. Gradually, however, intercourse became more normal...coitusbrought complete satisfaction to both ... this patient has aplasia of the vagina ... and under the influence of sexual life, the backfossae navicularisand front wallrectumstretched out, pulled into the rectum and formed a kind of vagina, quite suitable forcoitus ′ but».
She went to the doctor only because of the absence of children. In this situation, the reason for a fruitless marriage is easily explained.
In the practice of an obstetrician-gynecologist, there are even more "exotic" observations that explain the infertility of a woman.
Episode 7 Once, a woman close to our family, embarrassed, asked for help to determine the cause of infertility. More than a year of marriage, and pregnancy does not occur. I asked for a consultation with Prof. P.V. Manenkov. He always willingly responded to the requests of young employees. There was only one condition: it was necessary to initially try to figure out the diagnosis ourselves, and then invite him for a consultation. This time, I answered his short “Did you see it yourself?” in the negative, referring to deontology. Familiar, they say uncomfortable and something else like that. After carefully questioning the patient, he proceeded to the examination. At some stage, he suddenly asked me to move away to the side and began to quietly question the woman about something. I did not hear their conversation, but it was noticeable that the patient was unnecessarily worried. Having finished, as they say in the textbook, an additional anamnesis, he performed a rectal-abdominal examination and, briefly leaving “everything is fine”, let the patient go. He asked me to come into his office. Sitting down in a chair, he said:
-Your friends have a variant of dyspareunia.
I heard this term for the first time. Then, rummaging through the reference book, he found that “Dyspareunia is the general name for sexual disorders in a woman. Consists of "dys" (Greek) - prefixes mean "difficulty", "deviation from the norm", "impaired function". And "pareunos" (Greek) - sleeping with someone on the same bed, cohabitant (Encyclopedic Dictionary of Medical Terms. M., 1982, vol. I, p. 356).
– Your friend virgo. Their intercourse takes place between the closed thighs of the partner. I explained everything to her in detail. Don't forget to report the result.
“When the princess retired with him,
You would say that the night did not last long.
Filled with abundant dew -
A rose bud opened in the night
Drop by drop the rain streamed into the pearl
And pearls were born in the shell.
The darkness of the night has not yet thinned,
In the womb, this peri suffered.
And it all ended the same way, according to Ferdowsi:
“The circle of forty weeks has ended,
Like the sun, a son was born to a princess.
When I reported to the professor about the birth of Andryushka, he only smiled with satisfaction and enigmatism.
This is how we went through Gruzdev's school, marveling at the wisdom and delicacy of the Teacher.
P.S. When meeting, students always ask to tell something they remember in their more than half a century of work as an obstetrician-gynecologist. What has been said in this essay is only a small part of what has been experienced. Oddly enough, the cases most often recalled are not from obstetric and gynecological, but from general medical practice: one case of saving a 6-year-old girl from diphtheria croup, and the second - the restoration of hearing in a 70-year-old grandmother. Both are associated with the ENT specialty.
But more on that next time.
L.A. Kozlov, Doctor of Medical Sciences, Professor
Department of Obstetrics and Gynecology №1 KSMU
(head of the department - prof. Khasanov A.A.)
A foreign body of the uterus is the presence of a foreign object in the wall or cavity of the uterus. Quite often, intrauterine contraceptives (IUDs) or their parts (plastic hangers, metal fragments, threads), fetal bone fragments, surgical ligature and other foreign objects or fragments can be found in the uterine cavity.
Sometimes a foreign body in the uterus is encapsulated, and a long period of time does not make itself felt. True, often a secondary object can move under the influence of muscle contraction, migrate into the retroperitoneal space or abdominal cavity. As a result, perforation of the uterine wall occurs, which has a very negative effect on this organ. After infection of a foreign body, the uterus is affected by an inflammatory process that cannot be cured with active therapy.
In clinical gynecology, the timely removal and detection of foreign bodies of the uterus is of great importance. Otherwise, their presence can provoke the development of many dangerous complications.
Symptoms of a foreign body in the uterus
In most cases, the foreign body of the uterus is manifested by changes in menstrual function - spotting, metrorrhagia, menorrhagia. As a rule, a foreign fragment causes secondary infertility, chronic endometritis, and the development of pyometra. Initially, the uterus does not suffer from these items, everything changes with time.
If fragments of the IUD have entered the uterine cavity, this disappears without symptoms.
Pain can occur after the wall of the uterus is torn under the influence of parts of the IUD. After that, the particles can fill the entire cavity, the uterus will be subject to numerous injuries. The neighboring organ also suffers from this. The wall of the uterus can be completely perforated (the IUD extends beyond the uterine wall) and partially (the IUD is embedded in the myometrium). After that, a foreign object immigrates in the area of the omentum, bladder, rectosigmoid angle, appendicular process, retroperitoneal space, uterine appendages, small or caecum.
If we talk about the bone remains of the fetus, then they can be detected during examination of secondary infertility, menstrual irregularities, and prolonged endometritis. That is why it is recommended to carry out such a procedure regularly at least once a year. In this category of women, abortion is often observed for a period of 13-14 weeks, followed by repeated curettage of the uterine cavity and the appearance of bleeding.
Silk or lavsan ligatures are mainly detected in patients with pyometra, endometritis, gynecological or obstetric interventions (conservative myomectomy, caesarean section, etc.). This causes secondary infertility, purulent leucorrhoea, and the like. The uterus is severely damaged.
Diagnosis of a foreign body in the uterine cavity
In gynecology, the main method for detecting foreign bodies in the uterus is hysteroscopy. There are also other instrumental research methods (laparoscopy, examination on the chair, ultrasound, probing), but they are of an auxiliary nature.
A foreign fragment during a gynecological examination can be detected using a probe. Sounding has one significant drawback. With its help, it will not be possible to determine the exact location of the body, its size and shape, its relationship to neighboring organs and the walls of the uterus, its character, and the like.
To detect intrauterine contraceptives, transabdominal or transvaginal ultrasound is suitable, they are more informative. Fragments of the IUD often "attack" the uterine cavity or settle in the thickness of the myometrium. The ultrasound procedure is considered ineffective in the process of searching for bone remains and ligatures that have entered the uterine cavity.
The nature of the foreign body in the uterus has a decisive influence on the hysteroscopic picture. Foreign bodies, after a long stay in the uterus, can be covered with intrauterine synechia, endometrium and salts. In addition, these objects in the uterine wall can form bedsores in the uterine wall.
Only hysteroscopy allows you to determine the exact location of a foreign body. Without this research method, it is simply impossible to remove a foreign object, under the influence of which the uterus ceases to perform its functions over time.
Also in this process, a bacteriological examination of the smear plays a very important role. This technique is designed to select adequate antibiotic therapy. The sensitivity of the microflora to the drug is taken as a basis.
Plain radiography reveals foreign bodies located in the abdominal cavity.
Removal of a foreign body from the uterus
To remove foreign bodies from the uterus, special endoscopic instruments are used. With their help, foreign objects lying in the uterine cavity are purposefully pulled out through the hysteroscope canal. Some clinics practice the removal of foreign fragments without a hysteroscope, which is very dangerous. Such an operation can lead to deformation and fragmentation of foreign bodies, which will instantly provoke injuries to the walls of an organ such as the uterus.
Sometimes hysteroscopy is performed in combination with laparoscopy. This applies to situations where a complete or partial perforation of the uterine wall is detected.
Curettage of the uterine cavity is indicated in cases of ingrowth of foreign bodies into the thickness of the endometrium. As a result, the detected fragments will be deleted. As medical practice shows, sometimes to remove foreign bodies, doctors resort to colpohysterotomy (the uterus is dissected through the vagina).
If foreign bodies have gone beyond the uterus and penetrated into the abdominal cavity or neighboring organs, it is necessary to perform a laparotomy, and with a revision of the organs concerned.
There are cases when the presence of foreign fragments in the uterus causes massive infection and perforation. As a result, a hysterectomy is necessary. After the operation, antimicrobial treatment is prescribed to kill any infections that remain in the uterine cavity.
There is a special prevention of finding foreign bodies in the uterus, the essence of which is to carefully monitor the state of the uterine cavity, especially after abortion, removal of the IUD and gynecological operations.
A foreign body in the vagina is called absolutely any object that has entered the urogenital tract of a woman through the genital slit. Such a problem can cause inflammatory processes and the occurrence of various diseases: maceration of the skin of the perineum, pyoderma, endometritis, urethritis, cystitis, infertility, adhesions in the pelvis, intra-abdominal infection, tissue necrosis, injuries, fistulas and bedsores of the vaginal walls, injury to neighboring organs.
To avoid such troubles, for any symptoms indicating the presence of a foreign object in the vagina, contact a gynecologist at the Diana clinic.
How can a foreign body get into the vagina
A foreign body can get into the vagina under different circumstances:
- at the reception of a sloppy gynecologist, during examination or gynecological surgery;
- during sexual games;
- with injuries in the perineum;
- in the process of self-satisfaction;
- when terminating a pregnancy.
In addition, it can penetrate during manipulations related to contraception.
Symptoms of a foreign body in the vagina
After the foreign body has entered the vagina, the problem may not make itself felt for some time. The woman/girl then experiences the following symptoms:
- irritation;
- inflammatory process;
- hyperemia of the mucous membrane of the vestibule of the vagina;
- atypical discharge.
The doctor can confirm the fact that a foreign body is present in the vagina during a gynecological examination using mirrors. Additional methods may be required:
- two-handed research;
- colposcopy;
- vaginoscopy.
When a foreign body is found and removed, in order to exclude inflammatory processes, the gynecologist examines a smear from the walls of the vagina for the presence of bacteria.
If the doctor suspects that the foreign body has moved from the vagina, the patient is sent for a survey radiography, ultrasound, and computed tomography.
Removal of foreign bodies from the vagina
When removing a foreign body from the vaginal cavity, you must be extremely careful not to damage the walls of the vagina.
There are many tools with which a gynecologist can remove a foreign body from the vagina: urethral forceps, tweezers, a clamp with long narrow brushes, a Volkmann spoon. If something soft and fibrous gets into the vagina, vaginal lavage is used to remove it.
In severe cases, when the object has severely damaged the walls of the vagina or has shifted to the region of other internal organs, the patient is sent for a surgical operation, then therapy is applied, which consists in douching with various drugs.
In order to prevent the entry of foreign bodies into the vagina in girls, you should talk with them about the hygiene of the genital organs, follow their games. Vaginal products (hygienic or contraceptive purposes) should be used in accordance with the instructions.
More often than others, there are injuries that are produced by foreign bodies introduced into the genital tract for the purpose of fetal expulsion during criminal abortion. Such foreign bodies can be various probes, tips, knitting needles, wooden sticks, goose feathers, etc.
A foreign body, once in the external pharynx, can cause a neck wound, sometimes penetrating into the fiber, into the abdominal cavity; with retrodeviation, it pierces the posterior fornix and enters the cervical canal or even into the uterine cavity. It is believed that the cause of the majority of cervical-vaginal fistulas is not spontaneous central ruptures of the cervix during childbirth, but damage to the cervix during criminal abortions. The central ruptures of the cervix occur secondarily with cervical-vaginal fistulas, when the expulsion of the fetus occurs not through the external pharynx, but through the fistulous opening. As for fistulography, we believe that in women admitted for criminal abortion, suturing of fresh fistula openings should not be performed due to wound infection.
In the chronic stage of a fistula in non-pregnant women, suturing it does not always give a positive result. At subsequent births, when the fetus is born through a fistula, suturing a stretched fistula in a puerperal woman is advisable and gives better results than in non-pregnant women, provided that the cicatricial edges of the fistula are excised. However, not everyone agrees with this position.
Recently, Ya. E. Mesh described three cases of childbirth through a utero-vaginal fistula. The outer pharynx remained closed. The author believes that the fistula should be sutured after the first or second menstruation that occurred after childbirth.
In a significant proportion of cases, pointed objects introduced into the vagina were found not in the neck, but in the vaults, and they had to be removed. Leaving foreign bodies in the wall of the uterus or in the abdominal cavity for a long time can cause septicemia or peritonitis. If the instrument enters the uterus, then its wall is often perforated; at the same time, injury of the intestine or omentum and the development of peritonitis are possible. In such cases, urgent laparotomy is needed to remove the infected uterus, intestinal suture, or bowel resection.
The doctor can sometimes perforate the uterus during scraping of its mucosa. If perforation with a probe or a blunt curette is made after emptying the uterus, then sometimes you can do without surgery (prescribe 8 drops of opium three times a day). But in most cases, it is necessary to perform a laparotomy, remove the spilled blood, examine the intestines and omentum, and sutured the wound hole in the uterus after excising its edges.
Small objects that can slip into the uterine cavity or into the abdominal cavity are determined using x-rays. Depending on their location, the issue of intervention is decided: vaginal removal or laparotomy. To find foreign bodies, a digital examination of the uterine cavity may also be useful.